Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Unusual case of pulmonary artery dissection presenting as an exacerbation of COPD
Muhammad Najeeb Ullah Khan1,4; Hanady Hamdallah2; Aravind Ponnuswamy3*
1 Darul sehat Hospital, St-19, KDA Scheme, Abul Asar Hafeez Jalandhari Rd, Block 15 Gulistan-e-Johar, Karachi City, Sindh, Post code 75290, Pakistan.
2 Senior Lecturer, Chester Medical School, University of Chester, Bache Hall, Chester, CH2 1BR, UK.
3 Consultant Physician, GIM and Respiratory Medicine, Countess of Chester Hospital NHS Trust, Countess of Chester Health Park, Liverpool Road CH2 1UL, UK.
4 Shed Hospital, Plot No. St. 1, 2-A Sector 11 C 2 North Karachi Twp, Karachi City, Sindh, Post code 75850, Pakistan.
*Corresponding Author: Aravind Ponnuswamy
Countess of Chester Hospital NHS FT, Countess of
Chester Health Park, Liverpool Road, CH2 1U, UK.
Email: aravindpdr@yahoo.com
Received : Jan 20, 2022
Accepted : Mar 01, 2022
Published : Mar 08, 2022
Archived : www.jcimcr.org
Copyright : © Ponnuswamy A (2022).
Abstract
A 61-year-old male with a background of COPD and non-small cell lung carcinoma diagnosed ten years prior to presentation was seen with chest symptoms. He was an ex-smoker and presented with exertional dyspnoea, chest pain, cough, and wheeze. He had been on chemoradiotherapy for his cancer. The patient was seen in the clinic and admitted intermittently due to shortness of breath, pleural effusion, and exacerbations of COPD. He had undergone CT, MRI, PET scan and missed the PAD diagnosis due to post-chemo-radiotherapy effects. The patient was diagnosed with PAD incidentally through CTPA. The patient was treated medically throughout for Pulmonary hypertension. He was not fit for any surgical intervention and passed away approximately 21 months after diagnosis of Pulmonary artery dissection. The case highlight survival of months in a case of Pulmonary artery dissection without any intervention therapy, including surgery
Keywords: pulmonary artery dissection; post radiotherapy
Citation: Ullah Khan MN, Hamdallah H, Ponnuswamy A. Unusual case of pulmonary artery dissection presenting as an exacerbation of COPD. J Clin Images Med Case Rep. 2022; 3(3): 1721.
Background
Pulmonary artery dissection (PAD) is usually resulted as a complication of Pulmonary artery hypertension (PAH) due to chronic respiratory diseases like Chronic Obstructive Pulmonary Disease [1]. It is a rare, serious, and unfortunately a lethal disease [2]. Due to the acute death, many patients were diagnosed on autopsy [3]. However, recent technologies have enabled earlier diagnoses. In 1842, Helmbrecht described PAD for the first time [4]. The prevalence of PAD is 8 out of 109571 in autopsy samples [5]. Antemortem prevalence is not evident due to the rarity of the condition.
The typical symptoms of PAD are exertional dyspnoea, chest pain (retrosternal), cyanosis (central), and sudden haemodynamic instability [6]. However, Holzinger et al. presented a case report in 2010 of a 60 yr old male patient with idiopathic pulmonary artery dissection having no symptoms and treated surgically [1]. Its association after radiotherapy for Non-Small Cell Lung Carcinoma (NSCLC) has not been reported in the literature. This case will describe the first patient with PAD after chemoradiotherapy. Hence, in this report, we described the relationship of PAD secondary to chemoradiotherapy exposure in NSCLC patients and their survival up to months.
Case presentation
A 61-year-old male presented with exertional shortness of breath intermittent post-exertion chest pain in the clinic. The patient also had a mild cough with some brown sputum occasionally, but most of the time is white. The patient also complained that he had a wheeze, and after exertion or exercise, it triggers. The patient had no allergies. In addition, the patient had no nausea, abdominal pain, cyanosis, or other symptoms. The patient had a stage III non-small cell lung carcinoma and chronic obstructive pulmonary disease (COPD). The patient was on chemoradiotherapy for his NSCLC treatment. In addition, the patient was also on inhaled bronchodilators for COPD. He was a security guard by profession and was an ex-smoker accumulating 40 pack years. On examination, the patient had notable breath sounds on the right side of the lung, and it was normal otherwise. The patient had no lymphadenopathy and no clubbing associated with this. His abdomen was non-tender and soft. The physical examination was normal, with no other findings. The patient had obstructive spirometry with FEV1 of 1.5 lit (47% predicted) previously, and no further spirometry was attempted after the diagnosis of PAD. His echocardiogram confirmed Pulmonary hypertension with PAP of 40 mm of Hg normal sinus rhythm on electrocardiography (ECG).
The patient was diagnosed with an exacerbation of COPD. His radiological findings were left lung mass with a mediastinal shift towards left with clear right lung. The patient was treated with antibiotics, nebulizers, steroids, and oxygen. Followed by discharge on furosemide, warfarin, lansoprazole, salbutamol, Hypromellose eye drops, Seretide and ipratropium bromide inhaler. Two months later, the patient presented with pleural effusion and suspected malignancy. The patient had a CT scan, and the findings were the same as of 2014. The pulmonary functions were consistent with obstructive disease, i.e., FEV1 (40%), FVC (65%) and FEV1/FVC (47%). The patient was followed up with problems like pleural effusion, left lung collapse, suspected pulmonary embolism. CT revealed extensive emphysema disease for which long term oxygen therapy was set up at home at 2litres.
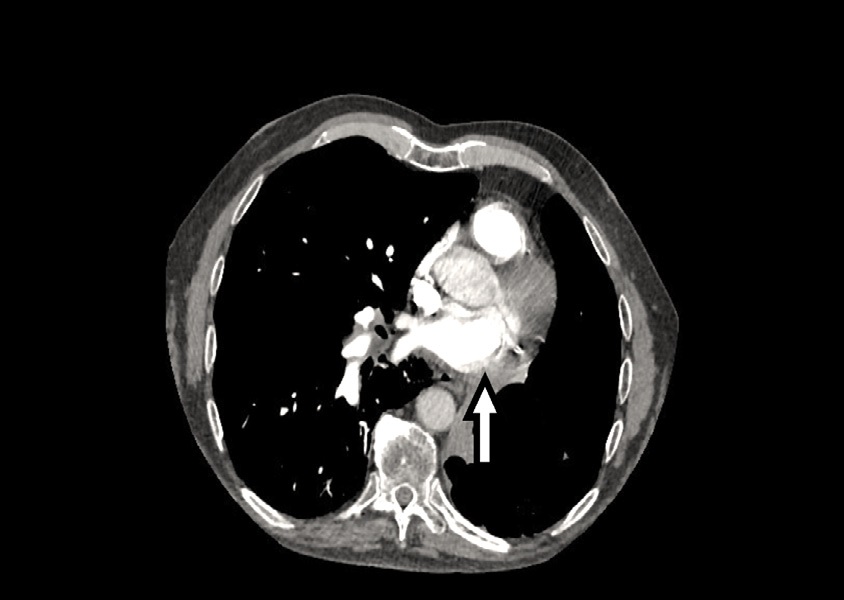
After six months, the patient again presented with occasional shortness of breath. Furthermore, due to recurrent exacerbations, a course of Augmentin and prednisolone was prescribed with a plan for azithromycin long term. A few days later, the patient was admitted in Acute and emergency with shortness of breath. On suspected pulmonary thrombus CT pulmonary angiogram (CTPA) was done, and the dissection of the main pulmonary trunk was revealed with extension to the left pulmonary artery (Figure 1). The patient was on tiotropium 20 microgram (1 puff/4 hourly), fluticasone salmeterol inhaler 500 (1 puff twice daily) and furosemide for his pulmonary hypertension. The cardiothoracic surgeons from the regional cardiothoracic centre were consulted, and it was decided to treat this patient conservatively. The patient was managed with antibiotics, nebulizers, and steroids for his acute presentation. The patient was discharged with a surgeon’s appointment on prednisolone doxycycline in addition to other ongoing medications. After the diagnosis was made, the patient had multiple follow up visits at the clinic to ensure his stable condition and adjustment in medication for COPD. Unfortunately, the patient also had multiple admissions due to exacerbations of COPD.
Discussion
Dissection of the pulmonary artery is rare [8]. PAD is an acutely fatal disease usually secondary to pulmonary hypertension with or without a pulmonary artery aneurysm (PA) [9]. However, it may be idiopathic and associated with inflammatory illness or trauma. Inayama, Y., et al reported 2 cases in their literature review. One patient with hypothyroidism had sudden dyspnoea and was treated by thromboendarterectomy for suspected pulmonary thrombosis. The second patient was diagnosed with PAD on autopsy. He was a known case of hypergammaglobulinemia and died due to a bleeding gastric ulcer [10]. This can be postulated that PAD can present as pulmonary thrombosis with dyspnoea like in this case. Cardiac malformation or congenital defects like Patent Ductus Arteriosus (PDA) are more associated with PAD which accounts for 66% of patients [11]. Wu, W. et al. did a study on ten patients; 9 were children and had PDA who developed pulmonary artery dissection, diagnosed on echocardiography [12].
Fernando, D. M. G., et al. reviewed 150 cases of pulmonary artery dissection, and they reported that the best investigation would be a CT scan which is a different approach from this case, i.e., diagnosed via CTPA. The authors described the chief causes of pulmonary hypertension and heart defects like patent ductus arteriosus compared to ventricular septal defect atrial septal defect [13]. They also found that females are more prone to develop PAD than males [13]. Pulmonary artery dissection with an aneurysm has rarely been described previously with amyloidosis, syphilis, endocarditis, valve surgery, tuberculosis, and connective tissue diseases like Marfan’s syndrome [14,15]. So, PAD is usually diagnosed by Echocardiography or CT chest, But in our case, the plain CT scan did not reveal the diagnosis due to post chemoradiotherapy changes and picked up on CTPA.
The clinical signs and symptoms of PAD are chest pain, exertional dyspnoea, cyanosis (central) and sudden shock/ collapse [10]. There could be murmurs if they were associated with heart valve defects. Our case did not have any cardiac c defects or valve abnormalities. However, patients with PAD may present without any symptoms or with a common symptom like dyspnoea due to some overlapping disease, for example, Exacerbation of COPD, as in our case. Walley, V. M., et al. suggested that PAD patients present with cardiogenic shock or acute death [16]. Pulmonary artery dissection led to sudden death due to the main trunk dissecting into the pericardium, causing cardiac tamponade [16]. Death is usually preceded by acute haemodynamic shock, which is described in previously stable patients [6]. In our case, the patient developed symptoms insidiously. The exact mechanism of PAD in our case is unknown. However, it can be hypothesized that the patient had received chemoradiotherapy, and the radiation could cause an arterial structure weakened and compounded by pulmonary hypertension. This patient was diagnosed after many visits and hospitalization through CT Pulmonary Angiogram (CTPA) and not readily on CT chest or PET scan.
The diagnosis of PAD during antemortem has been sparsely reported. PAD is the most reliably diagnosed by contrast computed tomography (CT) scan [13]. The cardinal signs of a CT scan are that the pulmonary tree can have a false lumen and intimal flap [17]. MRI can help diagnose PAD when the cause is heart defects [18]. In the chest x-ray, there will be pleural effusion and mediastinal widening signs (19). However, Lopez‐Candles, A. et al. described angiography as the gold standard for diagnosing PAD [6]. Therefore, it is essential to suspect pulmonary artery dissection in any patient with chest pain exertional dyspnoea with mediastinal widening.
This reported patient lived many months with the stability of condition after being diagnosed with pulmonary artery hypertension, which is very rare and unusual of its kind. Because approximately 86% of patients were diagnosed on autopsy [18]. This can be hypothesized that this patient might have a low degree of pulmonary hypertension after PAD due to previous chemo-radio therapy.
The early diagnosis of PAD is crucial and challenging for clinicians. Because of its atypical picture and pathogenesis. The physicians, pathologists and radiologists should be familiar with the diagnostic modalities, and once the diagnosis is made, the patient should receive emergency treatment to tackle this lethal and acute illness. The case highlights that the presentation of PAD may mimic the symptoms of another co-existing disease like COPD. It may not be associated with haemodynamic instability or systemic shock. Our patient survived up to a few months without any intervention
References
- Holzinger C, Podesser BK, Lomoschitz F, Kassal H. Idiopathic pulmonary artery aneurysm. Journal of cardiac surgery. 2011; 26(2): 154-6.
- Khattar RS, Fox DJ, Alty JE, Arora A. Pulmonary artery dissection: an emerging cardiovascular complication in surviving patients with chronic pulmonary hypertension. Heart. 2005; 91(2): 142- 5.
- Neimatallah MA, Hassan W, Moursi M, Al Kadhi Y. CT findings of pulmonary artery dissection. The British journal of radiology. 2007; 80(951): e61-3.
- Shilkin KB, Low LP, Chen BTM. Dissecting aneurysm of the pulmonary artery. The Journal of pathology. 1969;98(1):25-9.
- Kreibich M, Siepe M, Kroll J, Höhn R, Grohmann J, Beyersdorf F. Aneurysms of the pulmonary artery. Circulation. 2015; 131(3):310-6.
- Lopez-Candales A, Kleiger RE, Aleman-Gomez J, Kouchoukos NT, Botney MD. Pulmonary artery aneurysm: review and case report. Clinical cardiology. 1995; 18(12): 738-40.
- Perrotta S, Lentini S. Pulmonary artery dissection. Journal of cardiac surgery. 2015; 30(5): 442-7.
- Yamanaka S, Tanaka Y, Kawataki M, Ijiri R, Imaizumi K, Kurahashi H. Chromosome 22q11 deletion complicated by dissecting pulmonary arterial aneurysm and jejunal atresia in an infant. Archives of pathology & laboratory medicine. 2000; 124(6): 880-2.
- Senbaklavaci Ö, Kaneko Y, Bartunek A, Brunner C, Kurkciyan E, Wunderbaldinger P, et al. Rupture and dissection in pulmonary artery aneurysms: incidence, cause, and treatment—review and case report. The Journal of Thoracic and Cardiovascular Surgery. 2001; 121(5): 1006-8.
- Inayama Y, Nakatani Y, Kitamura H. Pulmonary artery dissection in patients without underlying pulmonary hypertension. Histopathology. 2001; 38(5): 435-42.
- Boyd LJ, McGavack TH. Aneurysm of the pulmonary artery: a review of the literature and report of two new cases. American Heart Journal. 1939; 18(5): 562-78.
- Wu W, Zhang N, Hsi DH, Niu L, Jiang Y, Wang Y, et al. Recognition of Ultrasound Artifact Mimicking Pulmonary Artery Dissection in Patients with Heart Disease. BioMed research international. 2019; 2019.
- Fernando DMG, Thilakarathne SMNK, Wickramasinghe CU. Pulmonary artery dissection—A review of 150 cases. Heart & Lung. 2019; 48(5): 428-35.
- Steingrub J, Detore A, Teres D. Spontaneous rupture of pulmonary artery. Critical care medicine. 1987; 15(3): 270-1.
- Arom KV, Richardson JD, Grover FL, Ferris G, Trinkle JK. Pulmonary artery aneurysm. The American Surgeon. 1978; 44(10): 688-92.
- Walley VM, Virmani R, Silver MD. Pulmonary arterial dissections, and ruptures: to be considered in patients with pulmonary arterial hypertension presenting with cardiogenic shock or sudden death. Pathology. 1990; 22(1): 1-4.
- Baptista R, Castro G, da Silva AM, Providência LA. Pulmonary dissection during diagnostic pulmonary angiography. Revista portuguesa de cardiologia: orgao oficial da Sociedade Portuguesa de Cardiologia= Portuguese journal of cardiology: an official journal of the Portuguese Society of Cardiology. 2012; 31(6): 465-465.
- Steurer J, Jenni R, Medici TC, Vollrath TH, Hess OM, Siegenthaler W. Dissecting Aneurysm of the Pulmonary Artery with Pulmonary Hypertension1• 2. Am Rev Respir Dis. 1990; 142: 1219-21.
- Wunderbaldinger P, Bernhard C, Uffmann M, Kürkciyan I, Senbaklavaci Ö, Herold CJ. Acute pulmonary trunk dissection in a patient with primary pulmonary hypertension. Journal of computer assisted tomography. 2000; 24(1): 92-5.