Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Iatrogenic aortocaval shunt treated by stent graft placement into the inferior vena cava
Peregrin JH1*; Vedlich D1; Šochman J2
1 Department of Diagnostic and Interventional Radiology, Institute for Clinical and Experimental Medicine, 14021 Prague 4, Czech Republic.
2 Department of Cardiology, Institute for Clinical and Experimental Medicine, 14021 Prague 4, Czech Republic.
*Corresponding Author: Peregrin JH
Department of Diagnostic and Interventional
Radiology, Institute for Clinical and Experimental
Medicine, 14021 Prague 4, Czech Republic.
Email: jan.peregrin@seznam.cz
Received : Feb 16, 2022
Accepted : Mar 08, 2022
Published : Mar 15, 2022
Archived : www.jcimcr.org
Copyright : © Peregrin JH (2022).
Abstract
Fifty six year old male sustained an injury to the abdominal aorta during his 1992 lumbar disc surgery with subsequent aortocaval shunt formation. In order to close the shunt, his abdominal aorta and both common iliac arteries were ligated and bilateral aortoiliac bypass was implanted. Postoperatively the patient remained asymptomatic for several years. Subsequently he developed arterial hypertension, his exercise capacity diminished and he complained of exertional dyspnea.
Intraarterial DSA demonstrated filling of the occluded aortic segment from intercostal and lumbar arteries as well and a shunt between this segment and the inferior vena cava. The hemodynamic significance of the shunt was confirmed using catheterization. Attempted reduction of the shunt flow by intercostal arteries embolization was not successful.
We were successful in closing the fistula using a custom-made stent graft.
CTA performed 18 years after the procedure confirmed absence of the shunt and patent inferior vena cava. The patient is now asymptomatic 23 years after the original surgery.
Citation: Peregrin JH, Vedlich D, Šochman J. Iatrogenic aortocaval shunt treated by stent graft placement into the inferior vena cava. J Clin Images Med Case Rep. 2022; 3(3): 1737.
Introduction
We present a case of a patient who during spinal surgery sustained an injury to his abdominal aorta with development of a hemodynamically significant aortocaval shunt. The shunt was initially unsuccessfully treated by aorta and both iliac arteries ligation and aortobiiliac bypass. Persistent shunt was later treated by placing a stent graft into the Inferior Vena Cava (IVC). The patient is now asymptomatic for 23 years after the procedure.
We present this case interesting due to the combination of an unusual aortic injury and non-standard treatment using venous stent graft.
Case report
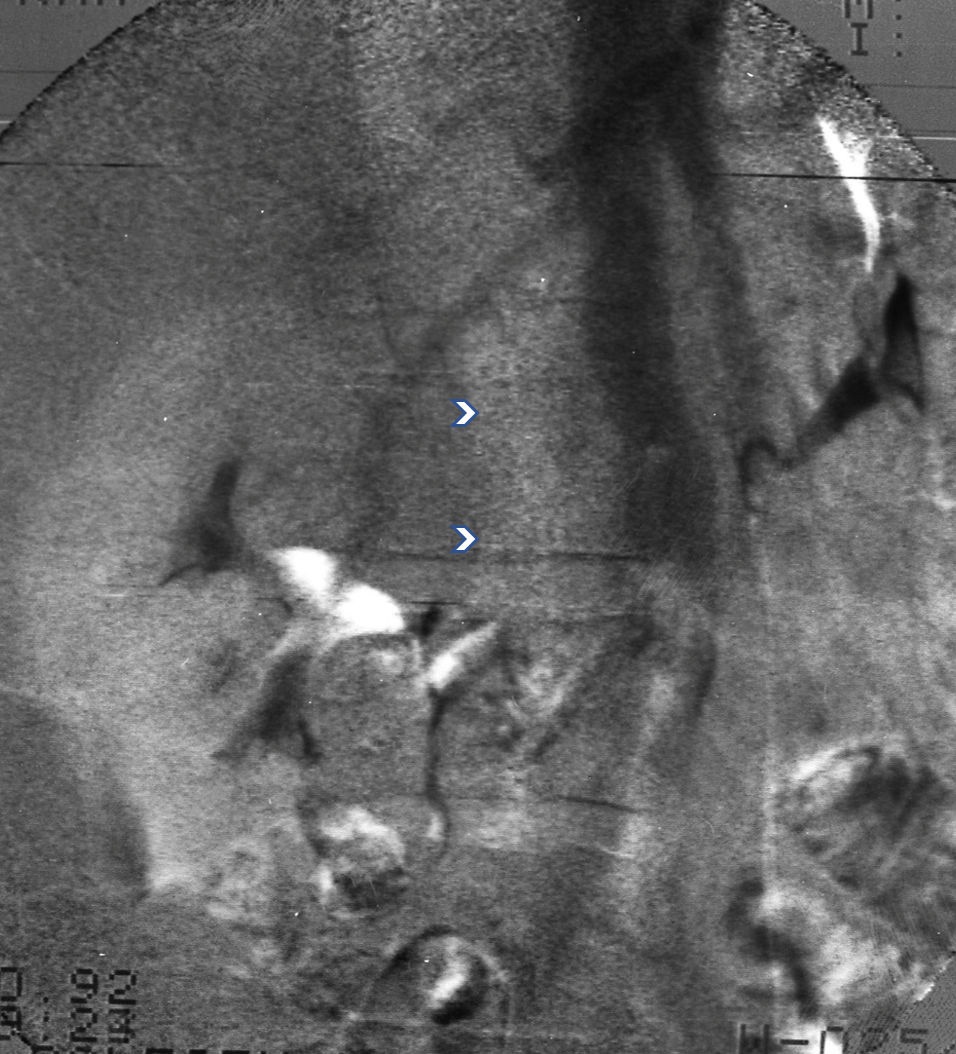
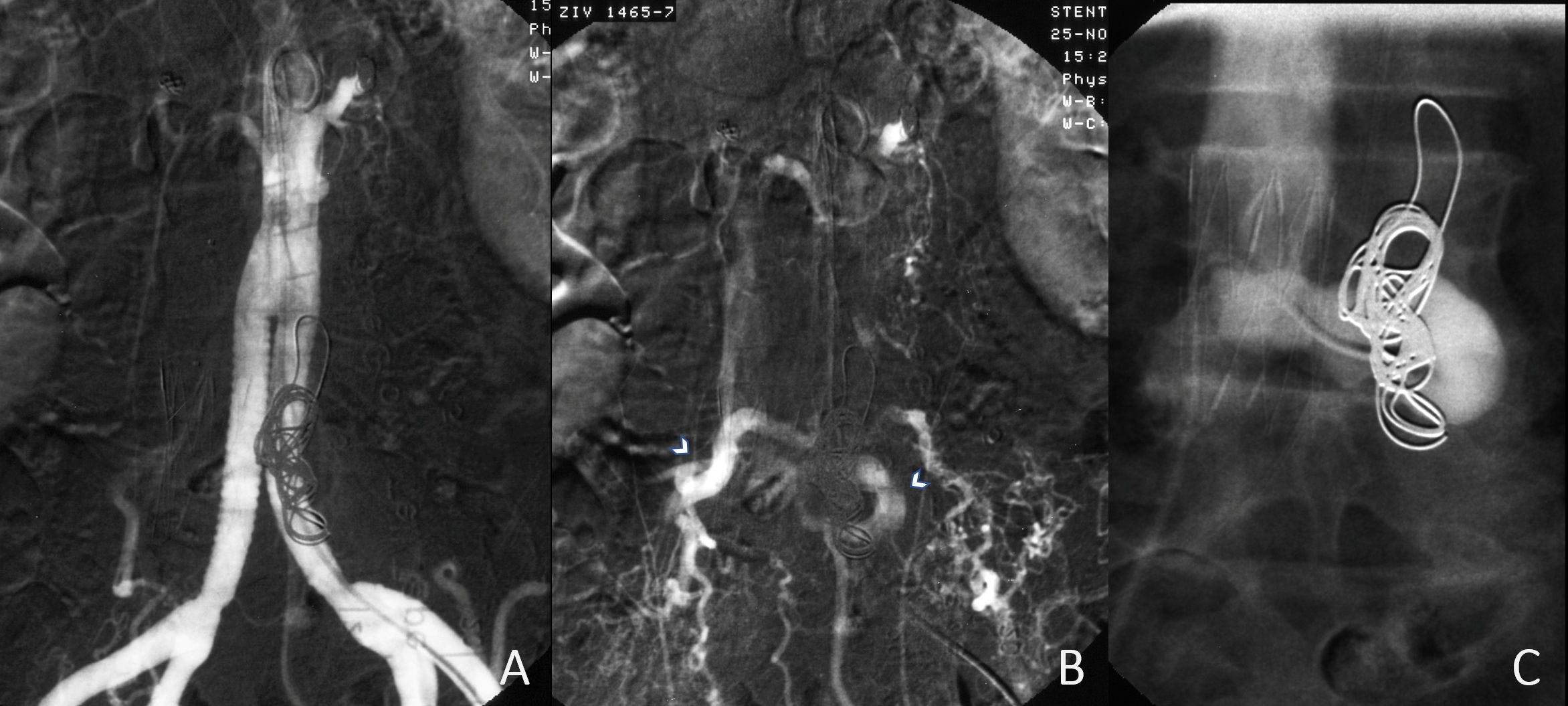
Fifty six year old male patient underwent in 1992 surgery for degenerative lumbar disc disease. Perioperatively he sustained injury to his distal aorta with subsequent development of an aorto-caval fistula. The complication was treated by ligation of the aorta and both common iliac arteries and bilateral aortoiliac bypass surgery. The patient was initially asymptomatic. At the request of the vascular surgeon intravenous Digital Subtraction Angiography (DSA) was performed. (The system was at that time only recently installed at our institution: Angiotron, Siemens, Germany, 256 X 256 matrix. The images were originally recorded on analog tapes and later digitalized) (Figure 1). The DSA image visualized patent aorto-biiliac bypass. It also showed almost simultaneous filling of the inferior vena cava (IVC). This was acceptable to the vascular surgeon. The visualization of the IVC was considered due to “over sensitivity of the DSA”.
Four years later (1996) the patient complained of decreased exercised capacity and exertional dyspnea. He also developed arterial hypertension. Physical exam was positive for a loud epigastric bruit.
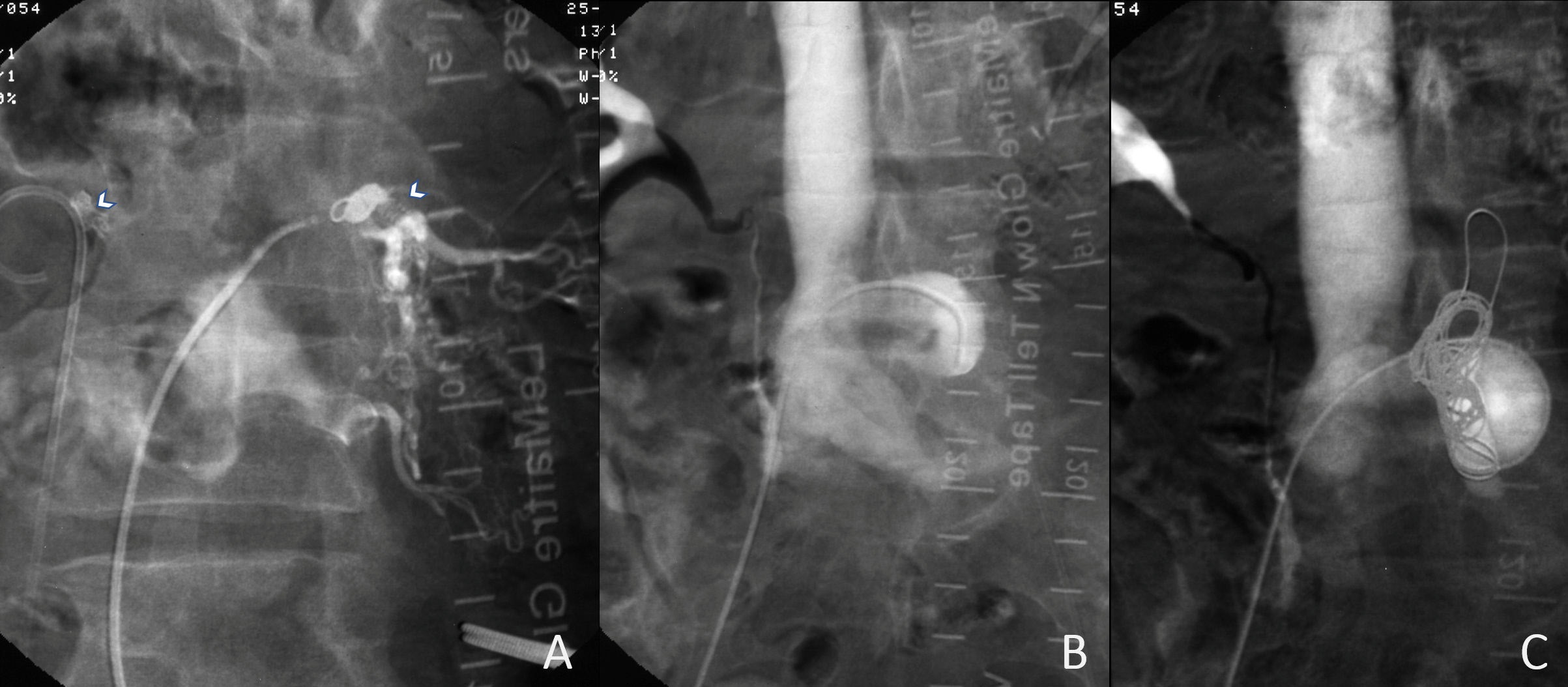
Intra-arterial DSA was performed using a fully digital system with a 1024 X 1024 matrix (Figure 2). A significant A-V shunt was seen at the level of the original aortic bifurcation draining dilated lumbar arteries as well as collaterals from the internal iliac arteries and the first lumbar and last intercostal arteries (Figure 2,3). After careful analysis we have determined that the angiogram showed a shunt between the aortic stump (distally to the aortic ligation) and the IVC.
Since the patient was clinically stable, conservative therapy using betablockers was continued.
In 1997 clinical examination was again positive for and bruit at the umbilical area. Cardiac echocardiography was normal (LV diastolic dimension was 57 mm).
In 1998 the patient, free of significant clinical symptoms, was hospitalized for shunt quantification. Echocardiogram documented hyperkinetic circulation and progression of left ventricular diastolic dimension (64 mm). Right heart catheterization revealed normal pressures in the right atrium and ventricle. Cardiac output was 8.7 l/min (CI of 4.04 l/min/m2 ). Oxygen saturation was 91% in the IVC, 74.5% in the SVC and 96.5% in the femoral artery. A nuclear angiography documented shunt flow of 60% of the total cardiac output. This alternative techniqueconfirmed hemodynamic significance of the shunt and need for therapeutic intervention.
Surgical intervention was considered but to be of a high risk. Instead, a percutaneous intervention consistent of closure of the shunt and IVC stent graft deployment was scheduled.
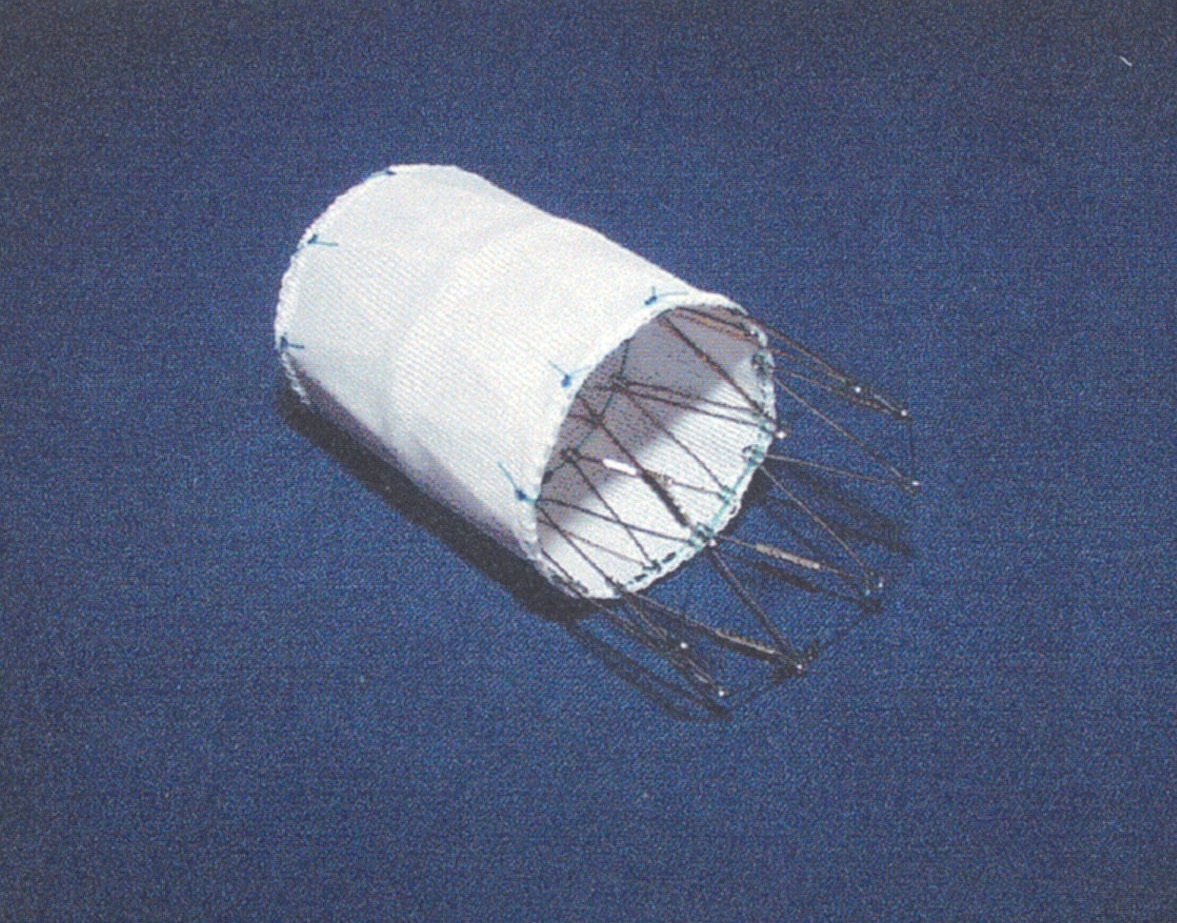
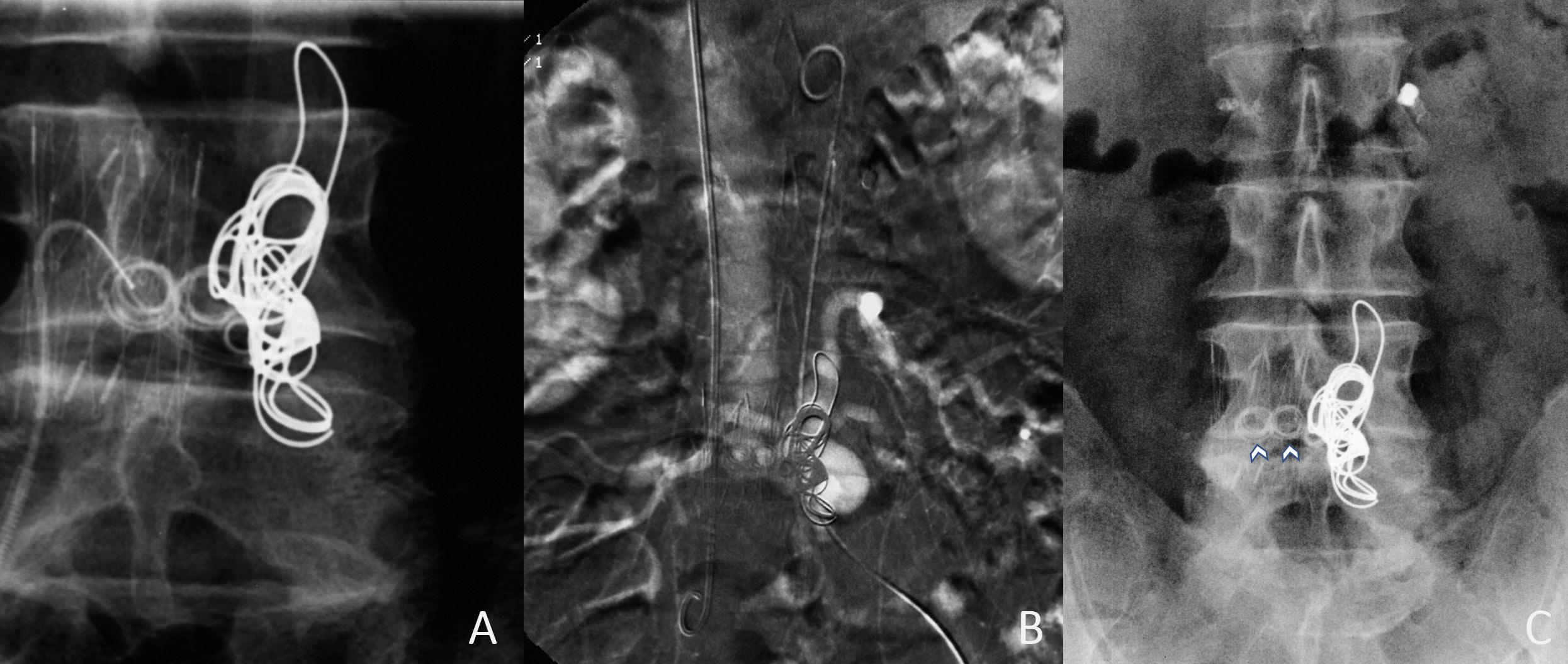
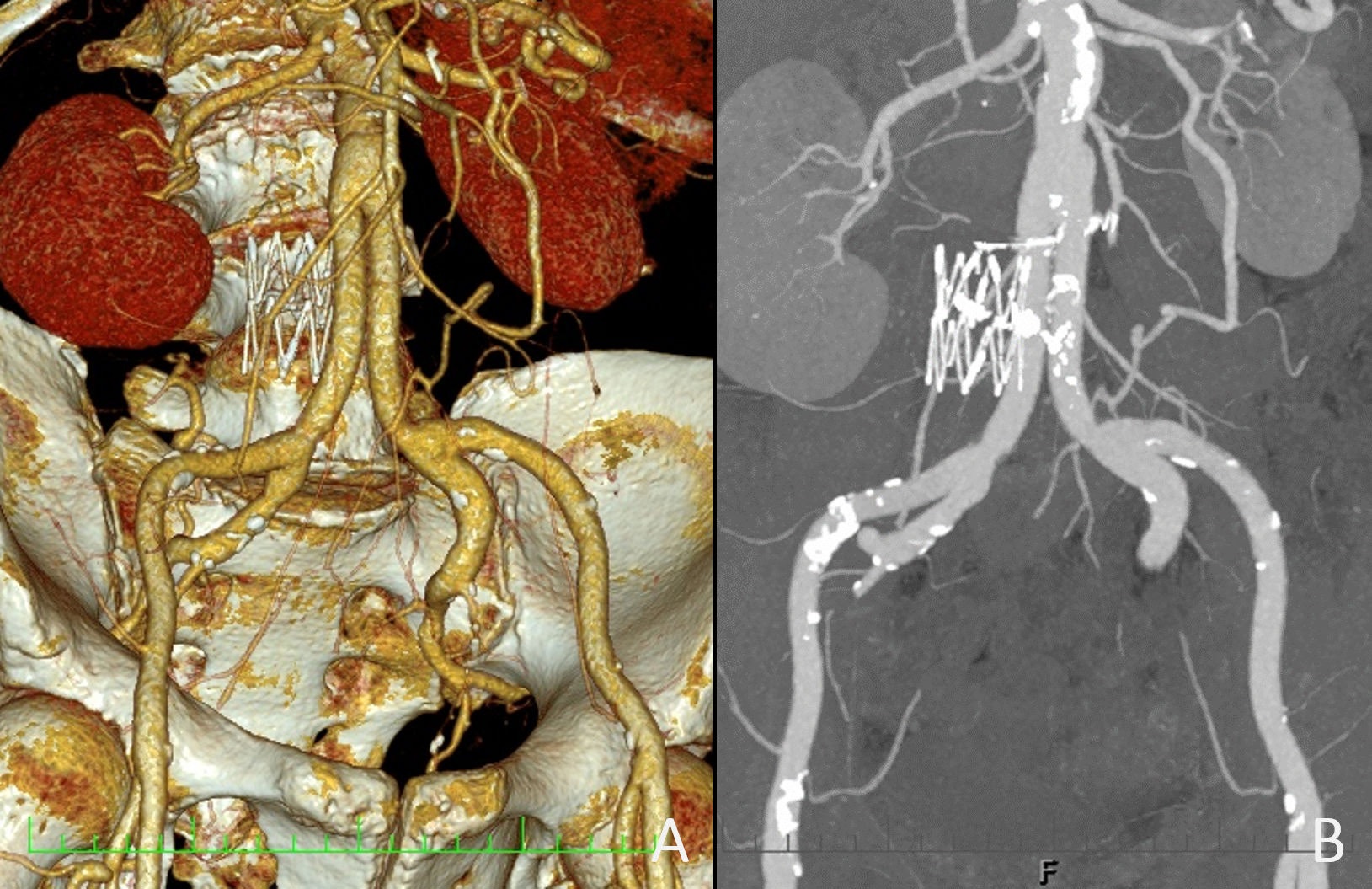
In preparation for the procedure, we customized and had locally manufactured (Ella, Hradec Kralove, Czech Republic) a stent graft fitting the IVC dimension (Figure 4). Prior to the stent placement, we inserted embolization coils Cook 4 mm/5 cm into the first lumbar arteries bilaterally in an effort to reduce the blood flow through the shunt; however, the effect on the flow was minimal as seen by angiography (Figure 5A). Next, using the right femoral venous access, we passed a Cobra catheter through the shunt to the aortic stump. Then we placed four 16 mm/30 cm Balt coils into the aneurysm located at the eycluded distal aorta (Figure 5B,C). Next, we placed the stent graft into the ICV at the site of the shunt (Figure 6). Follow-up angiography did not demonstrate shunt filling. The post procedural course was uneventful, the patient was discharged from the Hospital 3 days after the procedure.
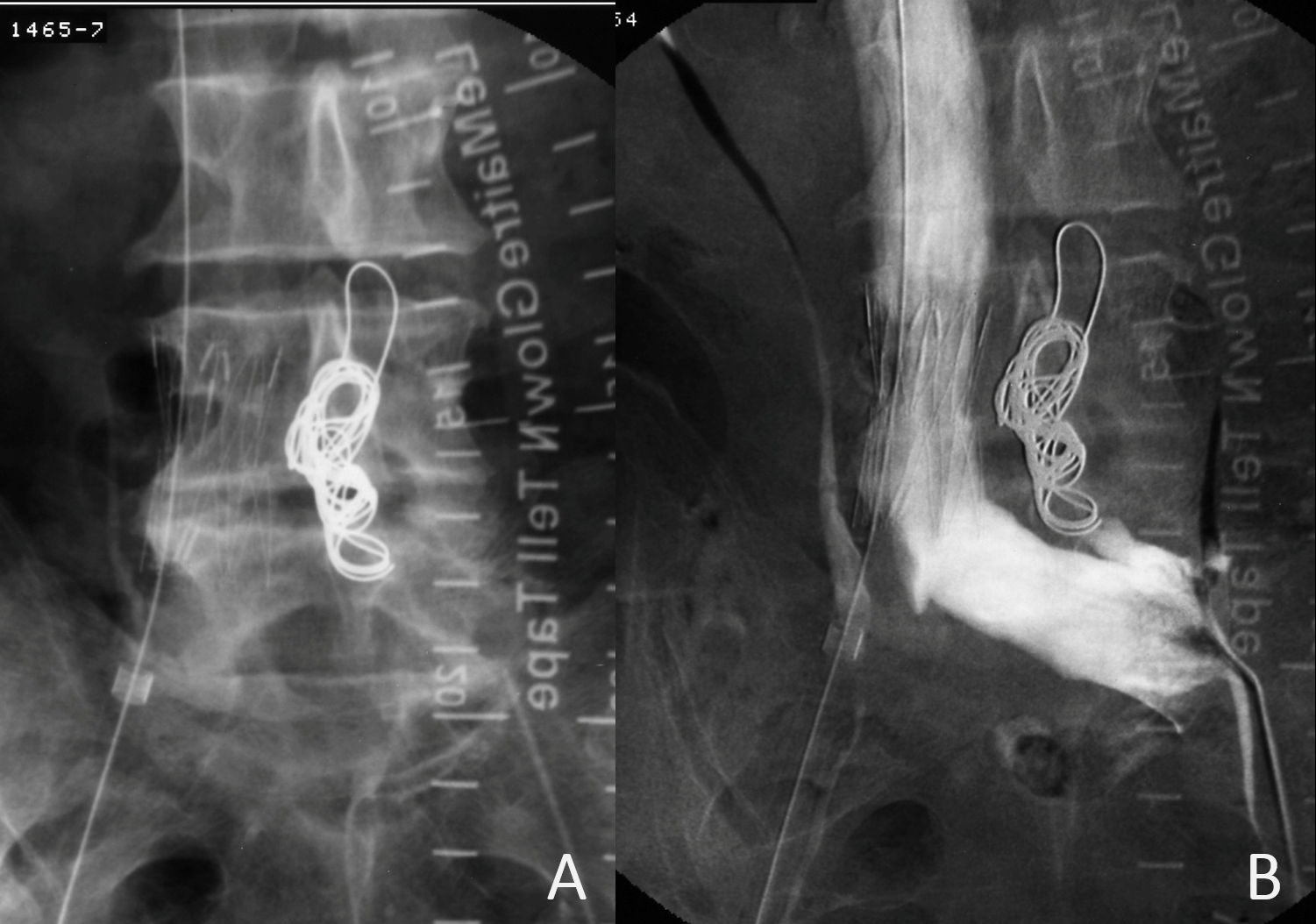
At the time of his 6 months follow-up visit a loud bruit was again audible at the umbilical area. Angiography detected presence of a smaller, but persistent shunt. In an attempt to close the shunt completely, we decided to place embolization coils between the covered segment of the stent graft and the wall of the original aorta. Using Simmons catheter, six COOK coils (four 5 cm/8 mm and two 6 cm/ 10 mm) were used. The shunt appeared to be completely obliterated.
During a follow- up visit a month later, no abdominal bruit was audible, echocardiogram confirmed absence of hyperkinetic circulation and return of diastolic left ventricular dimension to 58 mm. Right heart catheterization documented normal intracardiac pressures and absence of any significant differences in oxygen saturation levels as seen previously. Cardiac output was 5.8 l/min (CI of 2.7 l/min/m2 ).
The patient was lost to follow-up two years later (he moved to another region). In 2016 he presented to our hospital for an unrelated condition. Abdominal CT with contrast was done and demonstrated patent aortobiiliac bypass and absence of a shunt. Previously patent segment of the “original” aorta and previously hypertrophic lumbar/intercostal arteries were no longer visualized (Figure 9). The patient is now followed up yearly and remains asymptomatic.
Discussion
Aortic injury during lumbar spine surgery is rare, but several reports are available in the literature [1-3]. Depending on the injury morphology, bilateral aorto-biiliac bypass with exclusion of the damaged aortic segment has been used, similarly as has been done in our patient [4]. It is unclear why aortocaval fistula persisted after the surgery.
The DSA image was difficult to interpret since we did not expect the formation of the shunt from the excluded aorta. Also, the decision to place a stent graft was not easy since we had no previous experience with the procedure. In 1998 we used custom made stent graft of our own design which was locally manufactured. Currently we would most likely use a stent graft with shorter or none uncovered segment. Luckily the procedure was successful. It is unclear if the coil embolization between the graft and the IVC wall was necessary. Perhaps the procedure would have been successful even without the coil embolization.
At any rate, the strategy we opted for was most successful and effective for at least 18 years (time to follow-up CT) or even 23 years if considering clinical follow-up assessment.
References
- Fletcher JP, Klineberg PL, Hawker FH, Soni N, Woods WP, et al. Arteriovenous fistula following lumbar disc surgery-the use of total cardiopulmonary bypass during repair. Aust N Z J Surg. 1986; 56: 631-633.
- Görömbey Z, Gömöry A, Békássy SM. Iatrogenic aortocaval fistula secondary to intervertebral disc surgery. A case report. Acta Chir Scand. 1984; 150: 585-587.
- van Berge Henegouwen DP, Koopman MM, van der Werken C. Aorto-caval fistula after lumbo-sacral disc surgery. Neth J Surg. 1991; 43: 175-177.
- Woolley DS, Spence RK. Aortocaval fistula treated by aortic exclusion. J Vasc Surg. 1995; 22: 639-642.