Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Appendicitis in a drain-site hernia
Christopher Ashmore1*; Andrew Miller2; Daniel Couch3
1 ST3 General Surgery, North Lincolnshire and Goole NHS Trust, England.
2 Honorary Associate Professor of Colorectal Surgery, University Hospitals of Leicester NHS Trust, England.
3 ST8 Colorectal surgery, University Hospitals of Leicester NHS Trust, England.
*Corresponding Author: Christopher Ashmore
ST3 General Surgery, North Lincolnshire and Goole
NHS Trust, England.
Email: c.ashmore@doctors.org.uk
Received : Feb 07, 2022
Accepted : Mar 15, 2022
Published : Mar 22, 2022
Archived : www.jcimcr.org
Copyright : © Ashmore C (2022).
Abstract
A 73 year old woman underwent a Hartmann’s procedure for stricturing ulcerative colitis of the sigmoid colon. Following the procedure, she developed a tender, ruborous lump in the right lower quadrant, at the site of a recently removed silicone (Blake) abdominal drain. Computed tomographic images revealed herniation of the vermiform appendix in to the tract created by the abdominal drain. A diagnosis was made of acute appendicitis secondary to herniation of the vermiform appendix. The patient was managed conservatively with antibiotics, permitting the formation of an appendico-cutaneous fistula.
Keywords: appendicitis; abdominal drains; drain-site hernia; vermiform appendix; complications.
Citation: Ashmore C, Miller A, Couch D. Appendicitis in a drain-site hernia. J Clin Images Med Case Rep. 2022; 3(3): 1752.
Introduction
Surgical drains are a commonly used intervention to prevent the accumulation of fluids within a body cavity. Drain site herniae are an uncommon but significant complication of abdominal surgery with an estimated incidence of 0.1-3.4 % [1]. The most common organ of herniation is small bowel [1].
The presence of the vermiform appendix within a hernia is unusual however numerous cases have been described in the medical literature. Two well-known eponymous herniae are Amyand’s hernia, which describes an inguinal hernia containing vermiform appendix, and De Garengeot’s hernia, a femoral hernia containing the appendix. However, herniation of the vermiform appendix has been described in numerous locations including incisional [2] and spigellian herniae [3]. Appendicitis within a hernia sac is an extremely rare event and has a reported incidence of 0.008 % [4].
The herniation of an otherwise normal vermiform appendix in to a drain site has previously been described sporadically in several case reports [5-7], including two cases of evisceration of the appendix [8,9]. While appendicitis has previously been documented in port-site hernia [4,10], we describe what we believe to be the first reported case of acute appendicitis in a drain-site hernia.
Case report
A 73 year-old female patient attended the Emergency Department of a University Teaching Hospital complaining of one week of central, colicky abdominal pain, nausea and absolute constipation of 48 hours duration. She reported a background of well controlled asthma and ulcerative colitis, for which she took azathioprine and mesalazine. She had recently been prescribed a stool-softener by her General Practitioner to no effect. Abdominal examination revealed distension and left-sided tenderness with no evidence of peritonism. Blood samples and a venous blood gas were obtained. These revealed an elevated C-reactive protein and mild hyponatraemia only.
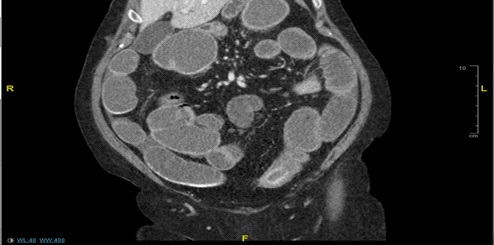
Computerised Tomographic (CT) images were obtained of the patient’s abdomen and pelvis. This revealed dilatation of both large and small bowel up to a thickened segment of mid sigmoid colon, concerning for acute stricturing ulcerative colitis (Figure 1).
An urgent surgical review by our out-reach general surgery consultant was quickly obtained. Following thorough assessment, it was found that the patient had no signs of peritonism and remained clinically well. The patient was catheterised, a nasogastric tube placed, and intravenous hydrocortisone and isotonic fluid prescribed. After a detailed discussion with a gastroenterology consultant, the patient agreed to a trial of medical management in the first instance. She was transferred to a gastroenterology ward and commenced on regular intravenous hydrocortisone and metronidazole. Further pre-biologic therapy screening tests were conducted which returned no significant findings.
Unfortunately, the patient did not respond to medical therapy and, following consultant surgical review, agreed to proceed with sigmoidectomy and end colostomy. The operation was arranged for the following day and the patient underwent an open Hartmann’s procedure, including the placement of a 14Fr silicone (Blake) drain in to the pelvis, exiting through the anterior abdominal wall of the right iliac fossa. The patient remained sedated and intubated for Intensive Therapy Unit (ITU) post-operative care.
The patient was cared for on ITU for three days in total, intubated for the first 24 hours. Following extubation, she became hypotensive, requiring copious intravenous fluids and noradrenaline. She developed a pyrexia, acute kidney injury and leukocytosis. A plain radiograph of the chest showed evidence of hospital acquired pneumonia and antibiotic therapy was commenced.
After three days, the patient was transferred to the ward for ongoing care. Unfortunately, she tested positive for SARS-CoV-2 on routine nasopharyngeal swab testing and was isolated in a side room, in accordance with Trust policy. On the ward, the patient became pyrexic and tachycardic, with worsening anaemia and metabolic derangement. She was treated for SARS-CoV-2 pneumonitis with a 9-day course of dexamethasone, oxygen titration and chest physiotherapy. Given that her colostomy was functioning well and her drain output was minimal, the decision was made to remove her abdominal drain. This was completed, without incident, by the nursing staff on the fifth post-operative day.
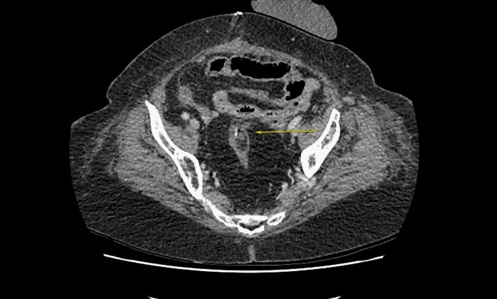
Unfortunately, the patient failed to improve, developing a tachycardia, pyrexia and raised inflammatory markers. Accordingly, a repeat CTAP was obtained, confirming the suspicion of a rectal stump dehiscence, without significant fluid collection (Figure 2). The patient was commenced on intravenous antibiotics and a rectal catheter was inserted for daily irrigation.
While recovering from SARS-CoV-2 infection and conservatively managed rectal stump dehiscence on the ward, the histology of the excised sigmoid segment was evaluated and reported. This confirmed the diagnosis of poorly differentiated adenocarcinoma (pT4a pN1a) of the sigmoid colon. A CT chest was obtained, which showed parenchymal ground-glass changes consistent with ongoing SARS-CoV-2 infection but no metastatic disease.
The patient remained on the ward for several days, receiving stoma training, nutritional assessment and electrolyte replacement. She failed to significantly improve, leading to further investigations including a vasculitis screen, wound swab and further CT evaluation. The patient was commenced on co-trimoxazole for a suspected wound infection following culture of Stenotrophomonas maltophilia, with limited effect, and transfused two units of packed red cells for a worsening symptomatic anaemia.
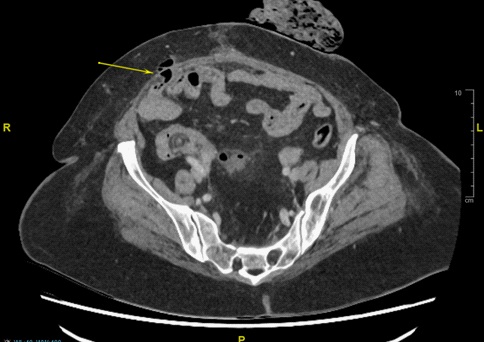
On the 27th post-operative day, a firm, tender, red lump of approximately 3 cm diameter was identified in the right iliac fossa of the patient, at the site of the pelvic drain. Previous CT imaging was re-examined and an opinion sought from a specialist GI radiologist. An addendum was added to the previous CT report confirming herniation of the tip of the vermiform appendix through the anterior abdominal wall at the site of the previously removed abdominal drain (Figure 3). Given the ruborous and tender nature of the identified structure, a clinical diagnosis of drain-site hernia appendicitis was established and the patient was commenced on intravenous antibiotics. After thorough discussion with the patient, it was felt that the safest management would be to adopt a non-operative approach, allowing the appendicitis to either resolve or fistulate through the abdominal wall.
The patient remained on the ward for a prolonged course of antibiotics but did not improve. There was concern that her clinical condition was the result of para-rectal collection as a sequalae of rectal stump dehiscence rather than appendicular abscess so additional CT evaluation was sought to characterise the patient’s abdominal pathology. This demonstrated relative stability of radiographic appearance of the rectal stump dehiscence but showed a fluid filled collection at the site of previous incarcerated appendix, indicating formation of appendicular abscess as a result of the drain-site herniation.
As expected, the patient developed an appendicocutaneous fistula (Figure 4). The wound was managed with skin protecting barrier creams and fashioning of an ileostomy bag for ongoing drainage of small volumes of turbid exudate. Following this fistulation, the patients clinical condition improved and her pain resolved. The patient was discharged with a prolonged course of antibiotics and early review at our Surgical Ambulatory Review Clinic. The patient did not attend her follow-up appointment but remains under the care of the colorectal multi-disciplinary team.
Discussion
The placement of drains following significant abdominal surgery remains a common surgical practice. Drain placement should not be considered a benign intervention as complications include wound infection, fistulation, intestinal obstruction and drain site-hernia. Factors which predispose to drain site herniae include increased intra-abdominal pressure, such as prolonged ileus or vomiting, use of large bore drains, local infection and patient comorbidity [11].
The presence of appendicitis in a hernia is a rare phenomenon and there exists no consensus on optimal management. Losanoff and Basson have described a classification for Amyandherniae which advocates for appendicectomy with herniorraphy in the presence of appendicitis and appendicectomy with Liechtenstein repair for a normal appendix [12]. However, there is general consensus that the use of prosthetic implant in any clean-contaminated procedure should be adopted with extreme caution. Both laparoscopic and open techniques have been described for the successful management of appendicitis in these hernia [12].
In this case, recent laparotomy in conjunction with poor functional status rendered further surgical intervention inadvisable.
References
- Makama JG, Ameh EA, Garba ES. Drain Site Hernia: A Review of the Incidence and Prevalence. West Afr J Med. 2015; 34: 62–68.
- Kler A, Hossain N, Singh S, et al. Vermiform appendix within incisional hernia. BMJ Case Reports. 2017; 2017: 221216.
- Peeters K, Huysentruyt F, Delvaux P. An unusual presentation of an incarcerated Spigelian hernia. Acta Chir Belg. 2017; 117: 312–314.
- Sugrue C, Hogan A, Robertson I, Mahmood A, Khan WH, et al. Incisional hernia appendicitis: A report of two unique cases and literature review. International Journal of Surgery Case Reports. 2013; 4: 256–258.
- Gass M, Zynamon A, von Flüe M, Peterli R. Drain-site hernia containing the vermiform appendix: Report of a case. Case Rep Surg. 2013; 198783.
- O’Riordan DC, Horgan LF, Davidson BR. Drain-site herniation of the appendix. Br J Surg. 1995; 82: 1628.
- Vuković M, Moljević N, Crnogorac S. Incarceration of the appendix into silicone drain holes without signs of appendicytis. Journal of Acute Disease. 2012; 1: 148–149.
- Byrne J, Kehoe JD, Kayyal MY. Special type trocar-site hernia with evisceration of the appendix following laparoscopic repair of a perforated duodenal ulcer. J Surg Case Rep. 2020; 2020: 376.
- Tidjane A, Tabeti B, Boudjenan Serradj N, Bensafir S, Ikhlef N, Benmaarouf N. Laparoscopic management of a drain site evisceration of the vermiform appendix, a case report. International Journal of Surgery Case Reports. 2018; 42: 29–33.
- Hassan TA, Shalaby H, Eskander A. Incarcerated appendicitis in port-site hernia: A rare case report. The Egyptian Journal of Radiology and Nuclear Medicine. 2015; 46: 569–571.
- Tonouchi H, Ohmori Y, Kobayashi M, et al. Trocar Site Hernia. Arch Surg. 2004; 139: 1248–1256.
- Ivanschuk G, Cesmebasi A, Sorenson EP, Blaak C, Loukas M, Tubbs SR. Amyand’s hernia: A review. Med Sci Monit. 2014; 20: 140-146.