Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Accidental discovery of appendiceal carcinoma in gynecological surgery: A case report and literature review
Lin Wang1*; Yan Dong1; Yahui Chen1; Yanan Wang1; Lin Sun2
1 Department of Clinical Medicine, Jining Medical University, Jining 272000, Shandong Province, China.
2 Department of Obstetrics and Gynecology, The Affiliated Hospital of Jining Medical University, Jining 272000, Shandong Province, China.
*Corresponding Author: Lin Wang
Department of Clinical Medicine, Jining Medical University, Jining 272000, Shandong Province,
China.
Email: wynjxj@163.com
Received : Mar 14, 2022
Accepted : Apr 04, 2022
Published : Apr 11, 2022
Archived : www.jcimcr.org
Copyright : © Wang L (2022).
Abstract
Objective: To introduce the common diagnosis and treatment of appendix cancer.
Methods: The discovery process and treatment plan of a patient with mucinous adenocarcinoma of appendix accidentally found in gynecological surgery in the Affiliated Hospital of Jining Medical College in May 2021 were summarized.
Results: The patient was treated for right lower abdominal pain and considered as ovarian tumor. Preoperative abdominal enhanced CT showed that the appendix was thickened. Cancer was found in the exploration of the appendix during gynecological surgery. The right colon was removed. After surgery, he received chemotherapy. At present, he has recovered well.
Conclusion: The incidence rate of appendiceal carcinoma is very low. Preoperative diagnosis is difficult. It is often found in operation or after operation. Preoperative examination and early evaluation of clinical manifestations are particularly important.
Keywords: Abdominal pain; Pelvic mass; Appendix carcinoma; Mucous adenocarcinoma.
Citation: Wang L, Dong Y, Chen Y, Wang Y, Sun L, et al. Accidental discovery of appendiceal carcinoma in gynecological surgery: A case report and literature review. J Clin Images Med Case Rep. 2022; 3(4): 1787.
Introduction
Malignant tumors of the appendix are extremely rare, Incidence in gastrointestinal tumors was less than 1%. The appendix epithelial malignant tumors can be divided into three categories, including Mucous Adenocarcinoma of Appendix (MAA), intestinal type of adenocarcinoma and signet ring cell carcinoma, Mucous adenocarcinoma of appendix is the most common histological type of the three groups, Its occurrence may be related to long-term inflammatory infiltration of the appendix. Preoperative diagnosis of appendiceal tumors is very difficult and is often diagnosed by pathology during or after appendectomy. Here we report a case of mucinous appendiceal adenocarcinoma accidentally found during operation due to right lower abdominal pain and pelvic mass, and review the relevant literature.
Case presentation
The patient, female, 49-year-old, visited our hospital for 3 days of right lower abdominal pain with nausea and vomiting. There was no alteration of the menstrual cycle. Gynecological ultrasound on May 15, 2021: A cystic, solid mass in the right adnexa area at approximately 6.2 cm X 5.6 cm X 5.8 cm in size, unclear right ovary, normal tumor markers (HE4, CEA, AFP), CA125 392.9 U/ml, CA199 88.27 U/ml, 2021-05-18 hypocystic shadow in the right adnexa area with visible compartment inside on complete abdominal CT and appendiceal thickening at maximal thickness of around 12 mm (Figure 1). The mass in the pelvic cavity was unidentified. Surgery was scheduled.
Treatment
Laparotomy exploratory on May 21, 2021: The right accessory and cystic mass were removed, thickening of the appendix (~6 cm in length and ~1 cm in diameter), with hard texture and edema, attached to the posterior wall of the ascending colon. Appendiceal malignancy could not be excluded. Rapid intraoperative pathology reported appendiceal malignancy. Right hemicolectomy and peripheral lymph node dissection were performed assisted by the Gastrointestinal Surgery. At the end of surgery, the residual intestine, stomach, liver, greater omentum and peritoneum surface were exploited and no evidence of abnormality was monitored.
Outcome and follow-up
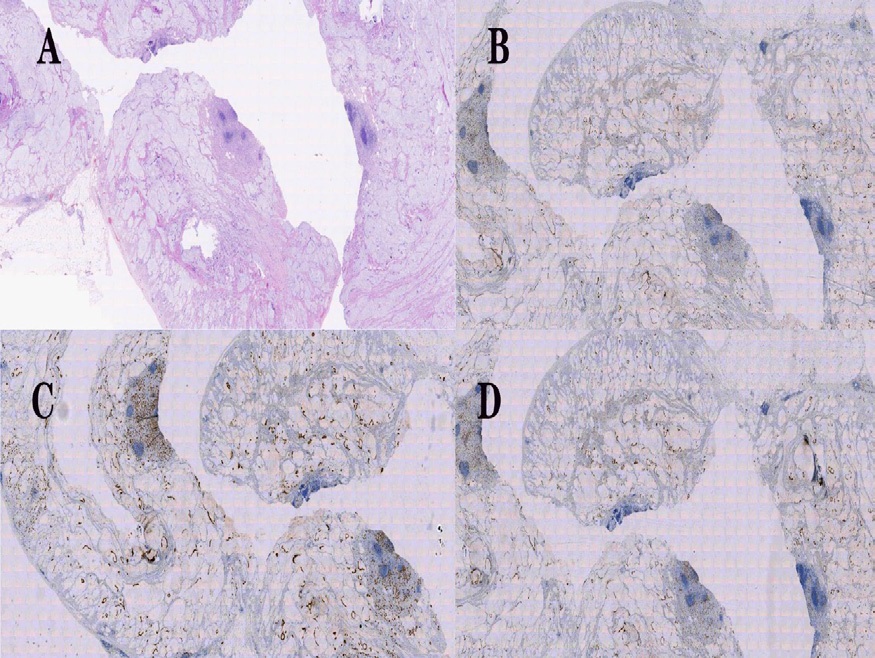
Postoperative pathology confirmed mucous adenocarcinoma of appendix with partial signet-ring cell carcinoma. Immunohistochemistry: CDX-2 (+), CK7 (-), CK20 (+), CA125 (-), CD56 (-), Syn (-), Pax-8 (-), WT-1 (-), SATB2 (+) (Figure 2). By now, 6 courses of XELOX chemotherapy regimen (Oxaliplatin + Capecitabine) were completed and there was no evidence of recurrence.
Discussion
MAA is a rare disease that generally occurs with elevation of CA199 and CEA. C.PABLO et al. revealed that tumor markers CEA and CA199 have high value in clinical application in diagnosis of mucous adenocarcinoma of appendix, and the increasing CA125 while normal HE4 help discriminate between benign and malignant ovarian tumors [1,2]. The patient reported here had elevation of CA199 and CA125, which is of certain value in diagnosis of appendiceal lesions [3]. Michelle Moh et al. combined immunohistochemistry to report common SATB (-), SATB2 (+) and CDX-2 (+) in ovarian mucinous tumors, highly indicative of the tumor being derived from the colon or the appendix [2]. Imaging is an important diagnostic method for mucous adenocarcinoma of appendix. Ultrasound findings may include cystic mass in the appendix, along with heterogeneous echogenicity, hypocystic or tubular lesions in the appendix as well accompanied by irregular thickening of the appendix. Appendiceal inflammation and abscess can be excluded by CT findings, and all the above findings help diagnose mucinous cyst [4,5]. MAA is hard to diagnose. Early symptoms lack specificity, mainly presented as lower abdominal pain, weight loss, nausea, vomiting, palpable mass and acute appendicitis, which are often mis-diagnosed with gynecological diseases, such as right adnexal mass [6]. The bladder can be also involved with signs of bladder irritation or occurrence of hematuria, leading to a mis-diagnosis with urinary tract infection or bladder cancer [7-9]. Iven the mentioned above, it is challenging to give a definite diagnosis of mucous adenocarcinoma of appendix. In most cases, appendiceal malignancy is detected accidentally by abdominal CT or surgery for appendicitis due to other reasons. Mucous adenocarcinoma of appendix is also a high risk factor of peritoneal seeding, hematogenous and lymph node metastases. Simultaneous surgical removal of the appendix and right hemicolectomy plus peripheral lymph node dissection [4,8], therefore, is preferred as a surgical treatment for mucous adenocarcinoma of appendix. Laparotomy is superior to laparoscopic operation as facilitating explore the involvement of other organs and better protecting the incision, in avoidance of mass rupture which can lead to intraperitoneal dissemination and affect prognosis.
Conclusion
MAA is highly rare and hard to diagnosis and differentiate from other tumors. It is vital significant to perform preoperative laboratory and imaging examinations and formulate welldesigned diagnostic and treatment strategy. Timely diagnosis and surgical treatment can significantly increase the long-term survival rate in patients [10,11]. The patient reported here manifested with common clinical symptoms of mucous adenocarcinoma of appendix, which, combining relevant literature, helps for early diagnosis of mucous adenocarcinoma of appendix in the future.
References
- Shin KH, Kim HH, Kwon BS, Suh DS, Joo JK, et al. Clinical Usefulness of Cancer Antigen (CA) 125, Human Epididymis 4, and CA72-4 Levels and Risk of Ovarian Malignancy Algorithm Values for Diagnosing Ovarian Tumors in Korean Patients With and Without Endometriosis, Ann Lab Med. 2020; 40: 40-47.
- Yan F, Shi F, Li X, Yu C, Lin Y, et al. Clinicopathological Characteristics of Pseudomyxoma Peritonei Originated from Ovaries, Cancer Manag Res. 2020; 12: 7569-7578.
- Wang B, Yao J, Ma R, Liu D, Lu Y, et al. The mutational landscape and prognostic indicators of pseudomyxoma peritonei originating from the ovary, Int J Cancer. 2021; 148: 2036-2047.
- A Van Hooser, TR Williams, DT Myers. Mucinous appendiceal neoplasms: Pathologic classification, clinical implications, imaging spectrum and mimics, Abdom Radiol (NY). 2018; 43: 2913- 2922.
- Tirumani SH, Fraser Hill M, Auer R, Shabana W, Walsh C, et al. Mucinous neoplasms of the appendix: A current comprehensive clinicopathologic and imaging review, Cancer Imaging. 2013; 13: 14-25.
- Ma Q, Wu J. Endometrioid Adenocarcinoma With Solitary Metastasis to the Appendix, Mimicking Primary Appendiceal Adenocarcinoma: A Case Report and Literature Review, Int J Gynecol Pathol. 2019; 38: 393-396.
- Roma K, Baldwin M, Sedmak D, Silva M, Stellar W, et al. Late stage diagnosis of mucinous adenocarcinoma of the appendix: A case report of an unusual tumor with a rare presentation, BMC Gastroenterol. 2020; 281.
- Subramanya D, Grivas PD, Styler M, Appendiceal carcinoma: A diagnostic and therapeutic challenge, Postgrad Med. 2008; 120: 95-100.
- Turaga KK, Pappas S, Gamblin TC. Right hemicolectomy for mucinous adenocarcinoma of the appendix: just right or too much? Ann Surg Oncol. 2013; 20: 1063-1067.
- Lu P, Fields AC, Meyerhardt JA, Davids JS, Shabat G, et al. Systemic chemotherapy and survival in patients with metastatic low-grade appendiceal mucinous adenocarcinoma, J Surg Oncol. 2019; 120: 446-451.
- Shaib WL, Assi R, Shamseddine A, Alese OB, C Staley, et al. Appendiceal Mucinous Neoplasms: Diagnosis and Management, Oncologist. 2017; 22: 1107-1116.