Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Do nasal angiofibromata only affect adolescent males?
Cheerag Bharatbhai Patel1,2*; Andrew Wood1,2,3
1 Department of Otolaryngology-Head and Neck Surgery, Waikato District Health Board, New Zealand.
2 Waikato Institute of Surgical Education and Research, New Zealand.
3 Waikato Clinical Campus, The University of Auckland, Waikato Hospital, New Zealand.
*Corresponding Author: Patel CB
Department of Otolaryngology-Head and Neck
Surgery, Waikato District Health Board,
New Zealand.
Email: cheeag.pat@gmail.com
Received : Apr 18, 2022
Accepted : May 20, 2022
Published : May 27, 2022
Archived : www.jcimcr.org
Copyright : © Cheerag BP (2022).
Abstract
We present the case, including imaging and histopathology findings, of a 62-year-old lady who presented with a short history of unilateral nasal symptoms and a unilateral nasal mass. Angiography and biopsy showed a vascular architecture akin to an angiofibroma. The tumour was therefore embolised before complete macroscopic surgical resection.
Juvenile Nasopharyngeal Angiofibroma (JNA) is a benign, extremely vascular tumour that classically affects adolescent males and accounts for approximately 0.05–0.5% of all head and neck tumours. There are reports in the literature of angiofibromata occurring in older patients of both genders, without the stereotyped anatomy, termed adult extranasopharyngeal angiofibroma (ENA). ENA is not however in the current WHO classification of head and neck tumours and as such there are no agreed histopathologic criteria for its diagnosis. This case further highlights the unusual range of sinonasal tumours and the need to maintain an open mind when treating vascular sinonasal tumours, in all age groups.
Citation: Patel CB, Wood A. Do nasal angiofibromata only affect adolescent males?. J Clin Images Med Case Rep. 2022; 3(5): 1856.
Introduction
Angiofibromata are benign vascular neoplasms comprised of abnormal blood vessels and fibrous tissue, their existence in the head and neck region is almost exclusively in the form of juvenile nasopharyngeal angiofibroma (JNA) [1]. One of several defining diagnostic features of JNA is the demography, typically presenting in adolescent males. To our knowledge, no case of adult extranasopharyngeal angiofibroma (ENA) has been reported in New Zealand. These vascular tumours are exceedingly rare in adults which can lead to delays in diagnosis and profound bleeding for the unsuspecting Otolaryngologist (ORL). In the New Zealand context, the first ORL doctor an adult with nasal obstruction or epistaxis meets may well be a Junior ORL registrar as was the case with this patient.
Case report
A 62-year-old female was assessed in an Otolaryngology (ORL) clinic with one month of left sided nasal obstruction and orbital proptosis. There was no pain, bleeding, or preceding trauma, and no ophthalmoplegia, vision impairment, or altered facial sensation. Her medical history included recent treatment for a stage IIIC (cT3N3M0) invasive pleomorphic lobular carcinoma of the left breast, including surgery, adjuvant radiotherapy and Trastuzumab. Flexible endoscopic examination revealed a large left nasal tumour. The right nasal cavity, nasopharynx, globe, cervical lymph nodes and cranial nerves were unremarkable on clinical examination. Several biopsies were carried out under topical local anaesthesia in the clinic room. This prompted brisk bleeding requiring nasal packing and hospital admission. This biopsy was considered non-diagnostic and a further biopsy was performed under general anaesthesia. Again, brisk bleeding was encountered and intravenous transfusion of three units of red blood cells was required owing to the severity of the bleeding. Cross sectional imaging revealed a 6.6 X 3.9 X 5.0 cm mass centred in the left nasal cavity with invasion of the anterior orbit, erosion of the left lamina papyracea, and extension into the left lacrimal sac.
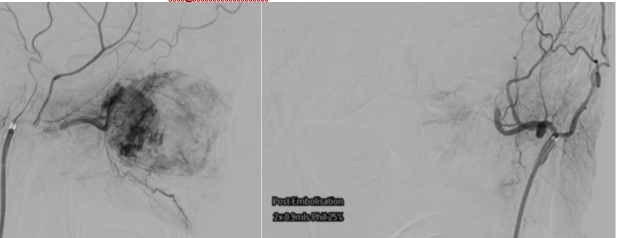
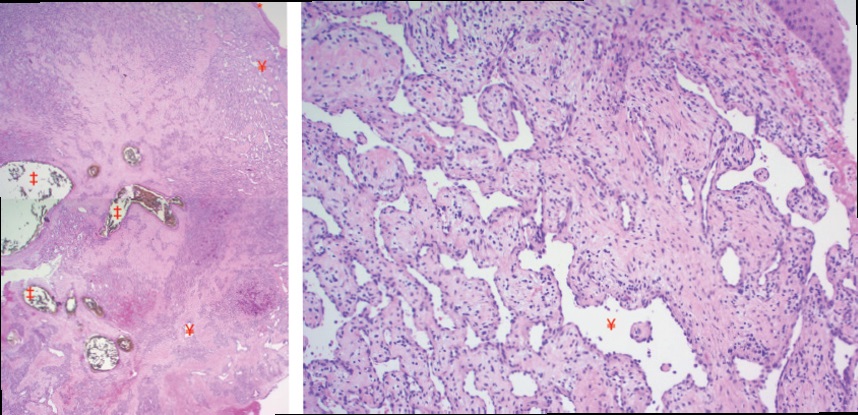
Microscopic examination of the biopsied tissue showed focal 56 fragments of inflamed, ulcerated, and necrotic tissue. Deep to these was a lobular proliferation of small vessels surrounded by a fibromyxoid stroma. No evidence of malignancy was seen. It was raised by the Pathologist that the microscopic features showed features of angiofibroma although on tertiary Pathology review the conclusion was of ‘benign sinonasal inflammatory or choanal-type polyp with angioectatic changes and infarction’. A digital subtraction angiogram and tumour embolisation was completed. Angiography (Figure 2) revealed supply from branches of the ophthalmic and ethmoidal arteries with an angio-architecture akin to an angiofibroma.
After embolisation, a transnasal endoscopic resection was completed. A deficient lamina papryracea was found but no direct invasion of the periorbitum and complete macroscopic tumour resection was attained. The patient was discharged from the hospital on the day after surgery with no packing in situ and a post-operative MRI has shown no evidence of persistent disease.
Discussion
This case highlights the importance of maintaining a wide differential diagnosis when treating sinonasal tumours. It is generally understood that the diagnosis of Juvenile Nasopharyngeal Angiofibroma (JNA) hinges on several features that come together to support the clinical diagnosis. These include typical demography (adolescent males), presentation (epistaxis, unilateral nasal obstruction), highly vascular nature, and typical origin from the sphenopalatine foramen.1 In JNA management, pre87 operative angioembolisation is now widely considered standard of care [1-3]. In the literature, a diagnosis of extranasopharyngeal angiofibroma (ENA) has been reported in a small number of cases, with clinical features that are not typical for JNA. There appears to be no clear age or gender exclusive preponderance such as in JNA. The site of origin also tends to be more variable, including the maxillary sinus, the ethmoid sinuses, part of the nasal cavity wall or even the nasal septum [4]. As highlighted by our Pathologist who therefore did not wish to make the diagnosis of ENA in this case, clear consensus has not however been reached regarding histological diagnosis of such tumours, hence the alternate diagnosis. The World Health Organisation’s classification of head and neck 97 tumours does not provide criteria for JNA-related or variant tumours such as adult ENA [5]. Several case reports of adult ENAs have reported similar histological features that were felt to be consistent with angiofibroma-like lesions. These features are abundant vascular channels of varying caliber, wall thickness and smooth muscle content admixed within fibromyxoid stroma with no evidence of atypia or malignancy [4,6-8]! Although this case was not typical for JNA, several features including the clinical behaviour and the marked internal vascularity on angiography were suspicious for an angiofibroma-like lesion. This was important in this case as it allowed us to consider angiofibroma in the differential diagnosis and plan accordingly. Pre-operative angioembolisation was an important determinant in the overall outcome, facilitating safe and complete resection with controlled bleeding, compared to the uncontrolled bleeding at the time of biopsy. Although a histological diagnosis of angiofibroma could not be made in this case, owing to the lack of agreed criteria, many of the features strongly support it. This case highlights the existence and importance of angiofibroma-like lesions in the context of adult nasal tumours and the importance of planning accordingly.
References
- Nicolai P, Schreiber A, Bolzoni Villaret A. Juvenile angiofibroma: Evolution of management. International Journal of Pediatrics. 2012; 2012: 1-11.
- Glad H, Vainer B, Buchwald C, Petersen BL, Theilgaard SA, Bonvin P, et al. Juvenile nasopharyngeal angiofibromas in Denmark 1981–2003: Diagnosis, incidence, and treatment. Acta Oto-Laryngologica. 2007; 127(3): 292-9.
- Gaillard AL, Anastácio VM, Piatto VB, Maniglia JV, Molina FD. A seven-year experience with patients with juvenile nasopharyngeal angiofibroma. Braz J Otorhinolaryngol. 2010; 76(2): 245-50.
- Bhagat S, Verma RK, Panda NK. Extranasopharyneal 130 angiofibroma in an adult: A rare presentation. Indian Journal of Otolaryngology and Head & amp; Neck Surgery. 2011; 63(S1): 25-6.
- El-Naggar AK, C. CJK, Grandis RJ, Takata T, Slootweg PJ. WHO classification of head and neck tumours. Lyon, France: International Agency for Research on Cancer (IARC). 2017.
- Mahmood AN, Sheikh R, Saey HA, Ashkanani S, Ganesan S. Angiofibroma originating outside the Nasopharynx: A Management Dilemma. Case Reports in Otolaryngology. 2016; 2016: 1-4.
- Stubbs VC, Miller LE, Parasher AK, Glicksman JT, Adappa ND, Palmer J. Nasopharyngeal Angiofibroma: A Forgotten entity in older patients. Clinical Medicine Insights: Case Reports. 2019; 12: 117954761984106.
- Nayak GK, Rawat PS, Kakoti A, Phookan J, Mitra R. Rare presentation of nasopharyngeal angiofibroma in adult. IOSR Journal of Dental and Medical Sciences. 2018; 17(6): 57-61.