Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Localized secondary amyloidosis of seminal vesicles associated with Von Willebrand’s disease: A case report and review of literature
Adishi Ranjan1; Alain Kaldany1; Evita Sadimin2; Hari Tunuguntla3*
1 Department of Urology, Rutgers Robert Wood Johnson Medical School, USA.
2 Cancer Institute of New Jersey, USA.
3 Department of Urology, Robert Wood Johnson University Hospital, USA.
*Corresponding Author: Hari Tunuguntla
Department of Urology, Rutgers Robert Wood Johnson Medical School, USA.
Email: tunuguha@rutgers.edu
Received : Apr 20, 2022
Accepted : May 23, 2022
Published : May 30, 2022
Archived : www.jcimcr.org
Copyright : © Tunuguntla H (2022).
Abstract
A 66-year-old man presented with a history of hypertension, benign prostatic hyperplasia (BPH), and urinary retention and multiple hospitalizations for gross hematuria with clots and clot urinary retention. A prostatic biopsy revealed localized amyloidosis of the seminal vesicles. The patient underwent transurethral resection of the prostate with postoperative clot urinary retention and gross hematuria. After it was resolved and the patient recovered, a postoperative hematologic evaluation revealed a diagnosis of von Willebrand’s diseases, a condition that results in bleeding diathesis from a mutated gene in the blood coagulation pathway involving factor VIII. This case of secondary amyloidosis of the seminal vesicles, along with gross hematuria and von Willebrand’s disease provides unique insight into the correlation between amyloidosis and blood coagulation abnormalities.
Keywords: Amyloidosis; Seminal vesicles; Von Willebrand’s disease; Hematuria; TRUS.
Citation: Ranjan A, Kaldany A, Sadimin E, Tunuguntla H. Localized secondary amyloidosis of seminal vesicles associated with Von Willebrand’s disease: A case report and review of literature. J Clin Images Med Case Rep. 2022; 3(5): 1859.
Introduction
Amyloidosis is characterized by the buildup of insoluble, fibrillar beta-pleated amyloid proteins within tissues that can lead to dysfunction or loss of function. The most common anatomical sites of amyloid buildup are the heart, kidneys, brain, and liver [1]. In the genitourinary tract, reported cases involve the testis, penis, prostate, ureters, kidney and seminal vesicles, with approximately half of those cases located in the urinary bladder [2]. Amyloidosis of the prostate and seminal vesicles is rare and can be detected by high levels of PSA (prostate-specific antigen) due to local inflammation or through TRUS (transrectal ultrasound guided biopsy) [3]. Amyloidosis can be classified as primary (AL) or secondary (AA), depending on the type of fibril that is deposited. Secondary amyloidosis, the more prevalent type, sees the deposition of amyloid A protein and a loss of affinity to Congo Red staining when treated with potassium permanganate [3]. Primary amyloidosis, interestingly, occurs in the absence of chronic inflammation. This condition within the genitourinary tract is exceptionally rare, with 1.5%-16% of cases occurring in the prostate, and a majority in the seminal vesicles and bladder [4,5]. Coagulopathy can also be seen in amyloidosis patients, typically due to a factor X deficiency or von Willebrand disease. As a result, hematuria can be a presenting symptom of amyloidosis, as 15-41% of patients experience excessive bleeding [6]. This paper details the unique case of a patient who initially presented with hematuria and was later found to have secondary amyloidosis of the seminal vesicles.
Additionally, postoperative bleeding after transurethral resection of the prostate was observed, and a new diagnosis of von Willebrand’s disease was made.
Case report
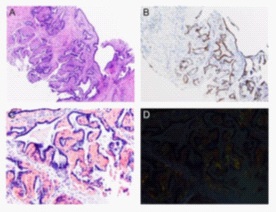
A 66-year-old man with a history of hypertension, benign prostatic hyperplasia (BPH), and urinary retention requiring indwelling Foley catheter placement presented with recurrent episodes of gross hematuria. He had multiple hospitalizations for hematuria, at times requiring clot evacuation and transfusion of blood products, and desired definitive surgical management of his BPH. Prior prostate biopsy showed benign prostatic tissue and localized amyloidosis of the seminal vesicles. Preoperative labs were notable for prolonged Partial Thromboplastin Time (PTT), however the patient was not seen by hematology prior to his procedure. The patient underwent a transurethral resection of the prostate with no intraoperative complications. Estimated blood loss was 50cc and complete hemostasis was achieved at procedure end. Intraoperatively, the resected tissue was noted to have a different gross visual appearance than typical hyperplastic prostatic tissue. The postoperative course was complicated by gross hematuria, clot retention, and subsequent anemia, eventually requiring a return to the operating room for cystoscopic clot evacuation and fulguration of the resection bed. During the second procedure, a large hematoma and areas of active bleeding were noted at the prostate resection bed, which were fulgurated. The hematuria subsequently resolved, and the patient recovered expectedly. Postoperative hematologic evaluation, including mixing studies and coagulation profile revealed a new diagnosis of von Willebrand’s Disease. Two out of seventeen biopsy cores showed pink amorphous extracellular material compressing branching glandular structure (Figure 1). The morphology, supported by PAX 8 immunostain and Congo Red stain, is consistent with seminal vesicles and amyloid deposition. Amyloid typing by liquid chromatography tandem mass spectrometry (LC MS/MS) revealed ASem1 (semenogelin 1). This type of amyloid deposition is generally localized to the seminal vesicles in older men. It is clinically inconsequential and has not been associated with systemic amyloidosis. The remaining fifteen cores showed benign prostatic tissue.
Discussion
The risk for amyloidosis of the seminal vesicles increases with age, with 21% of men over the age of 75 found to have seminal vesicle amyloid deposits [7]. Secondary Amyloidosis (AA) is typically associated with chronic inflammation, usually with conditions such as rheumatoid arthritis, chronic osteomyelitis, or malignancies [8]. This patient initially presented with hematuria, which is the most common symptom of amyloidosis of the urinary tract [8]. Amyloidosis can further be divided based on localized versus systemic. Localized amyloidosis (about 6-9% of all cases) remains confined to a single organ, whereas systemic amyloidosis is present in multiple anatomic sites [9]. Seminal vesicle amyloidosis is more common than prostate amyloidosis, though both can be characterized as localized rather than systemic disease [10].
Detection of amyloidosis occurs through Congo Red staining, the stain used for the demonstration of the amyloid protein in tissues. Congo Red binds to β-pleated sheets in amyloid proteins fibrils. In amyloidosis, the AA protein is denatured by the introduction of potassium permanganate through the alteration of its alpha sheet conformation, which indicates secondary amyloidosis, as the proteins associated with primary amyloidosis are resistant to denaturation. The fibril protein associated with amyloidosis of the seminal vesicle is ASem1, whose precursor protein is Semenogelin 1 [11]. This can be used in the identification and deposition of amyloid proteins on the target organ, seminal vesicles.
Coagulation is the process by which blood solidifies to establish hemostasis. Twelve clotting factors play a significant role in coagulation, and any disruption in these clotting factors can halt the coagulation process, manifesting as spontaneous or excessive bleeding. Amyloidosis has been associated with deficiencies in one or several coagulation factors, the most common of which is factor X deficiency, which has been reported in 8.7% to 14% of cases [12]. Although many factor X deficiency cases report systemic primary amyloidosis, we present a patient with factor VIII deficiency caused by localized secondary amyloidosis [12]. These clotting factors have an affinity for amyloid proteins, preventing clotting and resulting in a proclivity for bleeding [12]. Finally, treatments include replenishment of factor deficiency to rectify the blood coagulation pathway and prevent further bleeding or the reduction of amyloid with treatment with HDM/SCT[13]. There has been only one reported case of gross hematuria in a patient with secondary amyloidosis of the bladder [14]. Von Willebrand disease (VWD) is caused by mutations in the von Willebrand factor, affecting the carrier protein for clotting factor VIII [13]. A factor X deficiency is common, as stated above, however coagulopathy because of a deficiency in factor VIII makes this case unique.
Conclusion
We report the case of a localized, secondary amyloidosis of the seminal vesicles after transurethral resection of prostate. Additionally, our patient developed excessive postoperative hematuria after transurethral resection of the prostate that was noted to be secondary to von Willebrand’s Disease.
Declarations
Funding/support: All authors confirmed that the manuscript has not been and will not be published elsewhere or submitted elsewhere for publication. All figures of our manuscripts are original.
Conflicts of interest: All authors declare to have no conflict of interest. All Authors including confirmed that they have not any relevant financial interests or financial conflicts within the past 5 years and for the foreseeable future. They have no financial interests related to the material in the manuscript.
Ethical considerations: Authors declares that this study complies with current ethical considerations.
References
- Penelope P Scott, WWS Jr, Stanley S. Siegelman. Amyloidosis: An Overview Seminars in Roentgenology 1986. 21.
- Akram CM, Al-Marhoon MS, Mathew J, Grant CS, Rao TV. Primary localized AA type amyloidosis of urinary bladder: case report of rare cause of episodic painless hematuria. Urology 2006; 68.
- Lawrentschuk NPD, Stillwell R, Bolton DM. Implications of amyloidosis on prostatic biopsy. International Journal of Urology. 2004; 11: 925-927.
- Pitkänen, P., et al., Amyloid of the seminal vesicles. A distinctive and common localized form of senile amyloidosis. The American journal of pathology. 1983; 110(1): 64-69.
- Lupovitch, A., The Prostate and Amyloidosis. Journal of Urology. 1972; 108(2): 301-302.
- Sucker C, et al. Amyloidosis and bleeding: pathophysiology, diagnosis, and therapy. Am J Kidney Dis. 2006; 47(6): 947-55.
- Kawashima A, et al. Imaging evaluation of amyloidosis of the urinary tract and retroperitoneum. Radiographics. 2011; 31(6): 1569-82.
- Tolofari S, A Ansari, RJ Knight. A Rare Case of Hematuria; Primary Amyloidosis of the Bladder Neck. Urology case reports. 2017; 10: 48-50. DOI: 10.1016/j.eucr.2016.11.005.
- Singh SK, et al. Localized Primary Amyloidosis of the Prostate, Bladder and Ureters. International Urology and Nephrology. 2005; 37(3): 495-497.
- Nebil Bal NEK. Localized Secondary Amyloidosis of the Prostate. Journal of Urological Surgery. 2014: 51-52.
- Hazenberg BP. Amyloidosis: a clinical overview. Rheum Dis Clin North Am, 2013; 39(2): 323-45.
- Thompson CA. et al. Systemic AL amyloidosis with acquired factor X deficiency: A study of perioperative bleeding risk and treatment outcomes in 60 patients. American journal of hematology. 2010; 85(3): 171-173.
- Kos CA, et al. Association of acquired von Willebrand syndrome with AL amyloidosis. Am J Hematol. 2007; 82(5): 363-7.
- Boorjian S, et al. A rare case of painless gross hematuria: primary localized AA-type amyloidosis of the urinary bladder. Urology. 2002; 59(1): 137.