Journal of Clinical Images and Medical Case Reports
ISSN 2766-7820
Case Report - Open Access, Volume 3
Relevance intraoperative diagnosis of fibrous pseudotumor para testicular: Challenge for sparing testis
Elaouni Soukaina1,2*; Jebli Salma1,2; Sassi Samia1,2; Jahid Ahmed1,2; Zouidia Fouad1,2; Elkhanoussi Basma1,2; Bernoussi Zakia1, 2; Znati Kaoutar1,2
1Department of Pathology, Ibn Sina University Hospital, Rabat, Morocco.
2Faculty of Medicine and Pharmacy, University Mohamed V, Rabat, Morocco.
*Corresponding Author : Elaouni Soukaina
Department of Pathology, Ibn Sina University Hospital, Rabat, Morocco.
Email: soukaina_elaouni@um5.ac.ma
Received : Apr 18, 2022
Accepted : May 26, 2022
Published : Jun 02, 2022
Archived : www.jcimcr.org
Copyright : © Soukaina E (2020).
Abstract
A paratesticular fibrous pseudotumor is a relatively rare benign disease. Preoperatively diagnosing a fibrous pseudotumor is challenging because distinguishing these masses from malignant tumors on the basis of clinical and radiological findings is difficult to see impossible. We present a case of a 34-year-old man who presented with a 2-year history of right testicular swelling and was advised right radical orchidectomy by another surgeon. Physical examination revealed a painless palpable solitary mass in the right scrotum; Testicular tumor markers were all negative, and ultrasound scan showed a relatively hypoechoic lesion closely associated with the right testis and suspicious for neoplastic process. The patient underwent a testicular sparing surgery. An intraoperative frozen section biopsy confirmed the lesion to be benign and this was reported on permanent section to be fibrous pseudotumor of the tunica albuginea. Testicular-sparing surgery combined with frozen section assessment is primarily used for treating paratesticular fibrous pseudotumors.
Keywords: Paratesticular pseudotumor; Intraoperative diagnosis; Testis-sparing surgery.
Citation: Soukaina E, Salma J, Salma S, Ahmed J, Fouad Z, et al. Relevance intraoperative diagnosis of fibrous pseudotumor para testicular: Challenge for sparing testis. J Clin Images Med Case Rep. 2022; 3(6): 1866.
Introduction
Paratesticular fibrous pseudotumors (PFPs) are rare lesions thought to be reactive fibrous inflammatory hyperplasia. They originates from the tunica vaginalis, epididymis, tunica albuginea, or spermatic cord [1]. A PFP was first described by Balloch in 1904 [2]. PFPs constitute approximately 6% of all paratesticular lesions. Although they are common in the third decade of life, PFPs can be seen in all age groups. The pathogenesis and etiology remain unclear, however, these lesions usually develop after infection and/or trauma [3]. Patients mostly present with painless scrotal masses apart from the testicle. Ultrasonography (USG) is often sufficient to determine the lesions, and testicular tumor markers are useful to exclude malignancy. However, distinguishing these lesions from malignant lesions on the basis of clinical and radiological findings is still often difficult. Orchiectomies have been reported previously for the treatment of PFPs. Frozen section evaluation of the tumor is mostly recommended to avoid unnecessary orchiectomy [4]. Here, we present a case of PFPs to remind this uncommon condition, and, also to increase the awareness and knowledge with the support of a brief literature review.
Case report
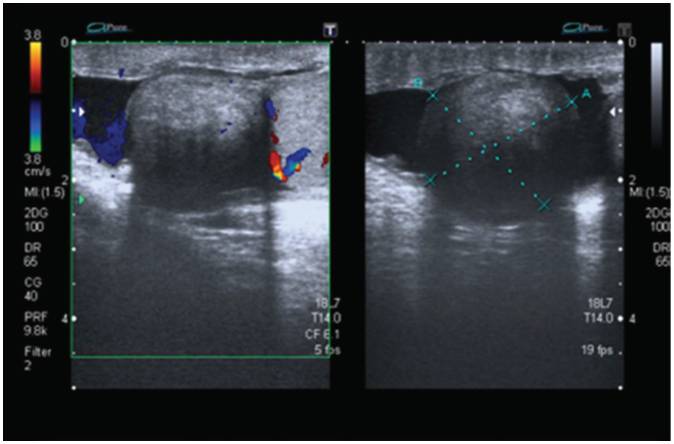
The complaint of our 34-year-old male patient was a painless scrotal mass. There was no history of trauma and/or epididymoorchitis. A round-shaped firm mass apart from the Right testicle was detected at the right side of the scrotum. There were no enlarged inguinal lymph nodes. His laboratory tests, including tumor markers for testicular cancer, were normal (alphafetoprotein: 0.95 μg/mL, human chorionic gonadotropin: 0.3 U/L, lactate dehydrogenase: 130 U/L) also the serum immunoglobulin level G4 (IgG4) was normal. Color Doppler USG of the scrotum revealed a paratesticular mass measuring 3,5 X 2 X 2 cm arising from the right testicular sac (Figure 1). The mass was excised through right inguinal incision. A solid, well-encapsulated mass originating from the epididymis was found during the surgical procedure. It was enucleated from the right testis, epididymis, and spermatic cord without harming them. The frozen section evaluation of the mass revealed a benign fibrous tumor. The gross specimen revealed a dirty-white firm mass, well-limited and unencapsulated with homogeneous and fasciculated appearance on the cut section (Figure 2). Histological control of the frozen section confirmed the diagnosis and showed a proliferation of typical fibroblasts that have been distributed multidirectionally bundles of dissociated collagen fibers, is associated with a slight inflammatory infiltrate of lymphoplasmacytic type (Figure 3). Immunohistochemistry demonstrated positive staining of the fibroblasts for smooth muscle actin (SMA), positive staining of the lymphoplasmoctic cells for CD138 and negative staining for CD34 (solitary fibrous tumor), desmin (leiomyoma), beta catenin (desmoid type fibromatosis), calretinin (mesothelioma) and anaplastic lymphoma kinase (ALK) (inflammatory myofibroblastic tumor). Also, based on our Ki-67 staining, the cell proliferation rate was low (Figure 4). No recurrences were detected at 10-month follow-up.
Discussion
A little more than 200 PFP cases have been reported. However, underreporting should be considered because of the complexity of the terminology and, also, confusing PFP with other pathologies. Various assigned names have been used for identification of this rare lesion [3]. PFPs can be seen in many age groups. The peak incidence is in young adulthood [2]. Therefore, PFP can be overtreated with orchiectomy with the testicular neoplasm prediagnosis. PFPs mostly originate from the tunica vaginalis [2]. PFP was originating from the tunica albuginea in our case.
Typical clinical presentation of PFP is slow-growing painless scrotal nodules. The diagnosis is mostly made by USG. Usually, the sonographic pattern is homogeneously hypoechoic lesion with sharp margins apart from the testicle. Magnetic resonance imaging (MRI) can be used to confirm the diagnosis. Typical findings on the MRI are intermediate signal density on T1-weighed and low signal density on T2-weighted images [5]. Also, heterogeneous gadolinium enhancement can be seen. We confirmed the diagnosis only by USG in our case.
Typical histopathological findings of PFP are plasma cells and lymphocytes interspersed between collagen bundles in hyalinized tissue [2]. Miyamoto et al. [6] subdivided PFPs into 3 categories on the basis of their 13 cases: [1] plaque-like; [2] inflammatory sclerotic; and [3] myofibroblastic [6]. Our case can be classified as group 2 according to this categorization. The differential diagnosis of PFPs includes solitary fibrous tumor, mesothelioma, neurofibromatosis, and leiomyoma. Histopathologic features (necrosis, pleomorphism, and increased mitotic activity), mostly specific to malignancies, are not found in PFPs. These features were not present in our case either.
Recently, it is suggested that paratesticular fibrous pseudotumor might be a part of IgG4-related sclerosing disease, which has an abundance of IgG4-staining plasma cells [7-9]. The diagnosis of IgG4-related disease is based on the combined presence of the characteristic histopathological appearance and increased numbers of IgG4+ plasma cells. The critical histopathological features are a dense lymphoplasmacytic infiltrate, a storiform pattern of fibrosis, obliterative phlebitis, tissue IgG4 counts, and IgG4/IgG ratios (approximately >40%) [10]. In addition, IgG4 elevation in serum may support the diagnosis. However, Ultrastructural evaluation has supported very minimal lymphoplasmacytic infiltration in our case and the serum immunoglobulin level G4 (IgG4) was also normal in our case .Unfortunately, histological IgG4 has not been evaluated in our case . Similar to our case, no etiological factor can be detected in most cases. Because the pathogenetic relevance of this test had not been considered during the clinical management, further studies are necessary to clarify the etiology of paratesticular fibrous pseudotumor.
Conclusion
PFPs are a rare clinic entity and can mimic malignancy, that is why to prevent unnecessary orchiectomy, testicular-sparing surgery combined with frozen section assessment is primarily used for treating paratesticular masses.
References
- Zhang Z, Yang J, Li M, Cai W, Liu Q, Wang T, et al. Paratesticular fibrous pseudotumor: a report of five cases and literature review. Front Med. 2014; 8(4): 484-48.
- Dieckmann KP, Struss WJ, Frey U, Nahler-Wildenhain M. Paratesticular fibrous pseudotumor in young males presenting with histological features of IgG4-related disease: Two case reports. J Med Case Rep [Internet]. 2013; 7(1): 1.
- Akbar SA, Sayyed TA, Jafri SZH, Hasteh F, Neill JSA. Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics. 2003; 23(6): 1461-1476.
- Kodama H, Hatakeyama S, Matsumoto T, Tanaka T, Horiguchi H, Kubota Y, et al. A Case of Fibrous Pseudotumor in the Scrotum: Challenge for Diagnosis and Testicular Preservation. Case Rep Urol [Internet]. 2018; 2018(c): 5-8. Available from: https://doi. org/10.1155/2018/6904827.
- Krainik A, Sarrazin JL, Camparo P, Vincendeau S, Houlgatte A, Cordoliani YS. Fibrous pseudotumor of the epididymis: Imaging and pathologic correlation. Eur Radiol. 2000; 10(10): 1636-1638.
- Miyamoto H, Montgomery EA, Epstein JI. Paratesticular fibrous pseudotumor: A morphologic and immunohistochemical study of 13 cases. Am J Surg Pathol. 2010; 34(4): 569-574.
- Dieckmann KP, Struss WJ, Frey U, and Nahler-Wildenhain M. Paratesticular fibrous pseudotumor in young males presenting with histological features of IgG4-related disease: Two case reports. Journal of Medical Case Reports. 2013; 7: 25.
- K. H. Kim, D. J. Sung, N. Y. Han et al. Immunoglobulin G4- related paratesticular fibrous pseudotumor and retroperitoneal fibrosis: A case report. Urologia Internationalis. 2015; 9(3): 369-37
- Bosmuller H, Von Weyhern CH, Adam P, Alibegovic V, Mikuz G, Fend F. Paratesticular fibrous pseudotumor-an IgG4-related disorder?. Virchows Archiv. 2011; 458(1): 109-113.
- Deshpande V, Zen Y, Chan JK. Consensus statement on the pathology of IgG4-related disease. Modern Pathology. 2012; 25(9): 1181-1192.